Terros Health inspires change for life by combining primary and behavioral health care
By DeEtte Person
Physical and mental health conditions used to be treated in silos. As a result, patients would see a doctor for one condition while another condition may have gone unnoticed. Today, that is beginning to change with organizations like Terros Health adopting behaviorally-led, integrated, whole health/whole person model of care.
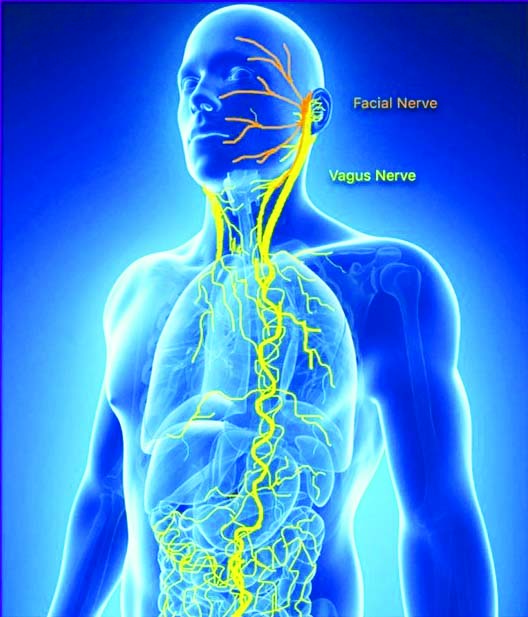
The model is exactly what it implies – caring for the body and mind as one
The whole health/whole person model changes the paradigm of care by helping physicians and other clinicians uncover a patient’s source of pain and evaluate alternatives to prescription drugs like cognitive behavioral therapy and mindfulness-based stress reduction. Patients and physicians work in partnership to treat not just a single ailment, but toward overall better health, physically and mentally. If there are signs of mental health issues or addictions of any kind, those can be dealt with in the earliest stages before they take a greater toll on a person’s physical health.
Behaviorally-led whole health/whole person care
This was true for Nicole, her husband Martin and their children who receive primary and behavioral health services through Terros Health at 27th Avenue Integrated Care. Nicole, was the first family member to seek out Terros Health to address grief due to the death of her and Martin’s 3-year-old son. The counseling she received helped and she began to go to Terros Health for her primary health care, as well.
Nicole encouraged Martin to give behaviorally-led integrated care a try. Today, the mental health care Martin receives has helped stabilize his depression and anxiety. He also receives excellent medical care for his diabetes. Their 20-year-old son Eric receives care from Terros Health’s behavioral health professionals. And, both Eric and 16-year-old daughter Mishelle are seeing primary care providers at Terros Health. Their older brother, Quinn, says he plans to reach out for his medical care.
For Nicole, she values the convenience of having all aspects of the family’s health care managed from a single location, including prescription refills. Without Terros Health and its integrated approach, she feels her family wouldn’t be doing nearly as well.
This success story is typical when integrated health care is implemented. By treating the whole person and weaving behavioral health into primary health care, even conditions such as diabetes and high blood pressure can have better outcomes.
Terros Health primary integrated care services include same-day or ongoing medical services including physical exams, chronic disease management, nutritional coaching, immunizations, lab work and prescription pick-up, all in one centralized location.
Treating the mind, as well as the body
The “whole health” approach also provides support for body, mind and soul when there is a mental health issue. Terros Health treatment programs are designed to be culturally-responsive and to coordinate with your overall health care plan. The health care team will support you every step of the way as you make choices — positive changes — that will put you on the path to true health and wellness for life. This includes counseling, treatment groups, crises services, psychiatric evaluations and medication management.
Karen experienced the whole health approach first-hand. As a child, Karen experienced sexual trauma in her family and again, at 19, when she was in the United States Naval Reserve (Women’s Reserve). Since then, she has struggled with nightmares, anxiety and depression. Karen tried to reduce her painful symptoms of post-traumatic stress (PTS) with alcohol, a common way to try coping with PTS.
While working as an early childhood educator in Hong Kong from 2008 through 2012 — in that busy and crowded metropolis – Karen’s PTS symptoms became overwhelming. She was unable to continue working and returned home to Phoenix. But her symptoms didn’t lessen.
A Terros Health crisis counselor recognized Karen had a bi-polar disorder, in addition to the alcohol use and PTS. She was referred to the Terros Health McDowell LADDER (Life-Affirming Dual Diagnosis Education and Recovery) program, located at the McDowell Integrated Care center, which helps people with co-occurring serious mental illness and addiction challenges by providing therapeutic behavioral health treatment and counseling that focuses on symptom reduction and management. Karen credits her progress to the support and education she received that makes it possible to deal with two of her issues at the same time. Today, she’s looking forward to returning to a position in early childhood education or becoming a peer support counselor to help others with similar challenges.
Optimizing health by treating addictions
Part of whole person care is regaining wellness by reducing alcohol, tobacco and other drug use, as well as risky sexual behaviors. Change can come in many forms — embracing new ideas, hobbies and healthy habits. At Terros Health, this involves counseling, detoxification, treatment and recovery support. In addition, one of the keys to success is engaging in life-affirming enrichment programs, such as life skills trainings and arts and cultural activities for youth and adults.
Robert knows well the success that can come from the support of integrated health care.
Robert stands well over six feet tall, and has the powerful physique of a body builder. Yet, inside his muscular body is a frightened little boy who experienced beatings no child should ever have to endure. When he was four years old his father, an alcoholic, drug user, biker and drug dealer, repeatedly beat him so severely he left permanent scars on Robert’s forehead. When his mother and father split up, things did not get any better for Robert. His mother’s new partner also was an alcoholic, and harshly disciplined Robert for things like not quickly memorizing multiplication tables in first grade.
In high school, Robert was free to rebel and rebelled badly, skipping school and using alcohol and pot. He dropped out of school and became, by his own definition, a “lazy pothead.” In his early twenties, things got little better for Robert. He got married, had a good job in a mill and limited his drug and alcohol use to weekends. But after four or five years, the marriage broke up because Robert started “using” more than just on weekends. Finally, the law caught up to him and he was sentenced to seven years in prison.
Robert remarried after he got out of prison, but he still needed treatment. He made the decision to become part of Terros Health’s Maverick House. There, he confronted his alcohol and drug addiction. And perhaps most importantly – for the first time – he came to terms with the violence he experienced as a child.
The day Robert graduated from treatment at Maverick House was the day he also decided to keep his recovery going by living at Maverick House Sober Living. At Sober Living, he has a healthy environment of 27 caring men committed to supporting each other and living positive lives without alcohol or drugs. Robert’s wife lives nearby and they have a positive relationship. But, Robert’s home — for now — is Sober Living, because that is where he has the structure and the fellowship of men committed to supporting each other in recovery.
Integrated care can provide key to treating an epidemic
Integrated health care creates healthy communities by providing welcoming “one stop shops” for the needs of a person’s mind and body. In turn, this leads to what is known in health care circles as the Triple Aim – an excellent customer experience, quality care outcomes and controlled health care costs.
A patient’s integrated health care team will include a primary medical care provider and may include mental health care providers, community health workers, a case manager, wellness/prevention coach and counselors. All elements of care are coordinated across the broader health care system including specialty care, hospitals, home health care, community services and other supports. The team works together to anticipate patients’ needs, communicate findings and to ensure no aspect slips through the cracks.
A good example of how integrated health care can heal an individual, family and even community is when it comes to the opioid epidemic. This dangerous class of drugs includes prescription pain relievers such as oxycodone and hydrocodone. You might have been prescribed these after a surgery, even one as minor as wisdom teeth removal. But did you know this same class of drugs also includes heroin? On the street, heroin is cheaper – hence the revival of heroin addiction, overdose and death.
Opioids are destroying lives in cities and states throughout the nation. Arizona is no exception. Sadly, two people in our state died every day from prescription opioid or heroin overdoses last year. All told, opioid overdoses claimed the lives of 790 Arizonans in 2016 – a 74 percent increase since 2012.
If you or anyone in your family has been prescribed these medications, talk to your physician about precautions to take. Following an integrated health model like that adopted by Terros Health can help doctors identify the signs of drug use and abuse in their early stages – signs such as drowsiness or sedation, slurred speech, uncharacteristic problems with attention and memory and constricted pupils.
If you would like experience to experience the transformative power of integrated health care, or if you need mental health or addiction care services, please call Terros Health at 602-685-6000. www.terros.org
DeEtte Person is a freelance writer living in Scottsdale, Arizona