Kristen Polin proudly identifies as a member of the recovery community and remains a fierce advocate for eradicating the stigma surrounding mental health and all addictions. She is the CEO of notMYkid, an Arizona nonprofit dedicated to prevention and behavioral health for youth and families, and a mom of two teen boys. Her daily mantra? “One day at a time, one hour at a time, one breath at a time. Whatever works. Just stay.”
Remembering the tipping point with alcohol
If you are someone who identifies as being in recovery, do you remember when you initially crossed the very first tipping point into addiction? That moment when the imaginary line was crossed from social and “normal” use to a place of needing something to feel normal or comfortable in your own skin?
I remember. It was a deep knowing inside when I was still a teenager that something had shifted, and it scared the heck out of me. I ignored that knowing for a very long time, until I couldn’t. Many people can relate to that instinctual tendency to deny it, even when the gut-level knowing stays in the background noise. Fast forward to today and all I can say is — I’m one of the lucky ones that finally figured out how to live one day at a time and overcome an addiction I have secretly battled on and off for decades.
I’m grateful for my dear friend, Barbara Brown, who created space for me to share my story about alcohol and shed light on alcohol use disorder (AUD) as a recovering woman, a mom, and as a dedicated professional in the behavioral health industry for over 25 years. Not all of those years were spent sober or in recovery, so I’m sharing a bit of my journey in the hopes that it brings awareness and a safe space for others to break their silence and shatter the shame and stigma that keeps people from getting the right help at the right time.
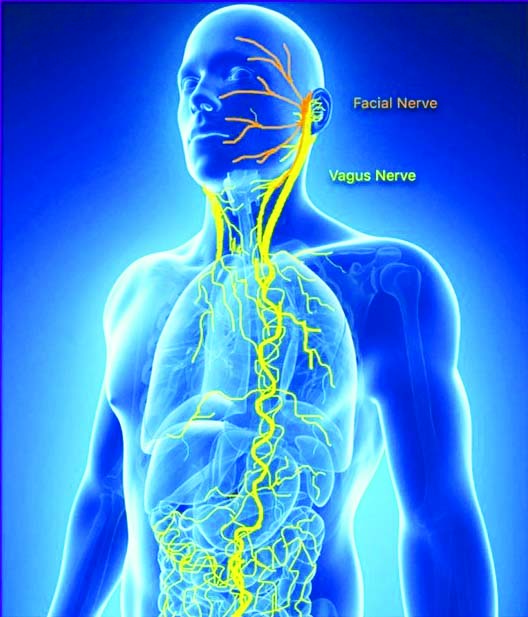
Early on in my recovery I learned that addiction is also a disease of isolation, and that the opposite of addiction is connection.
Connection is where healing begins
It’s no wonder two years beyond the start of the pandemic, we are continuing to learn more about the toll this experience has had on people of all ages and all walks of life. Read on and please keep sharing your stories of hope and recovery as often as you can. There is no better time to be of service and help others realize that recovery is possible.
April is Alcohol Awareness Month
Today and all throughout the month of April, the prevention and behavioral health community dedicates resources and education to shine a spotlight on problem drinking and raise awareness about alcohol use disorder. It’s important to balance accurate information and resources alongside a gigantic industry that normalizes social drinking and ingrains alcohol use as a normal way of life in our society. Rarely does it portray the negative impact on our health and the implications that alcohol use disorders can have on an individual, their loved ones, and our community?
Alcohol remains the most widely used and abused drug and became a much bigger issue for so many during the pandemic. We have witnessed three battles roaring alongside a public health crisis that escalated mental health challenges and suicide; fueled the opioid and fentanyl crisis, and alcohol-related deaths surpassed COVID-19 deaths for adults under the age of 65 in 2020.
I personally cannot fathom where my life may have been if I didn’t have my sobriety and recovery community intact when COVID-19 first arrived. It has been a tough two years. It was even harder for individuals who may have already been struggling prior to the pandemic. We know them. They are/were loved ones, co-workers, and friends.
Just how bad did it get? Alcohol-related deaths in the U.S. rose 25% from 2019 to 2020. According to research recently published by the Journal of the American Medical Association, pandemic-induced stress and delayed treatment contributed to the major spikes in death. Alcohol-related liver disease was the top underlying factor, followed by overdoses from alcohol, along with overdoses of other drugs where alcohol was involved. The largest spike on record was among 35–44-year-olds.
Defining an Alcohol Use Disorder and when it goes beyond problem drinking
According to the National Institute of on Alcohol Abuse and Alcoholism (NIAAA), an alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. Considered a brain disorder, AUD can be mild, moderate, or severe on the spectrum. The good news is that no matter how severe the problem may seem, evidence-based treatment with behavioral therapies, recovery support groups, and/or medications can help individuals achieve and maintain recovery. But make no mistake. We have A LOT of work to do since the pandemic impacted access to quality care for an extended period of time.
What Increases the Risk for AUD?
First, I always share that anyone is at risk because addiction is an equal-opportunity affliction. According to the NIAAA, a person’s risk for developing AUD depends on how much, how often, and how quickly they consume alcohol. Alcohol misuse, which includes binge drinking and heavy alcohol use over time increases the risk of AUD.
Other factors also increase the risk of AUD:
Drinking at an early age. A recent national survey found that among people ages 26 and older, those who began drinking before age 15 were more than 5 times as likely to report having AUD in the past year as those who waited until age 21 or later to begin drinking. The risk for females in this group is higher than that of males.
Genetics and family history of alcohol problems. Genetics play a role, with hereditability approximately 60 percent; however, like other chronic health conditions, AUD risk is influenced by the interplay between a person’s genes and their environment. Parents’ drinking patterns may also influence the likelihood that a child will one day develop AUD.
Mental health conditions and a history of trauma. A wide range of psychiatric conditions—including depression, post-traumatic stress disorder, and attention deficit hyperactivity disorder—are comorbid with AUD and are associated with an increased risk of AUD. People with a history of childhood trauma and adverse childhood experiences (ACE’s) are also vulnerable to AUD.
Symptoms Checker for AUD
When is the meter or that tipping point headed from mild, to moderate, then severe? Healthcare professionals use criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), to assess whether a person has AUD and to determine the severity if the disorder is present. Severity is based on the number of criteria a person meets based on their symptoms—mild (2–3 criteria), moderate (4–5 criteria), or severe (6 or more criteria).
A healthcare provider will ask the following questions to assess a person’s symptoms.
In the past year, have you:
Had times when you ended up drinking more, or longer, than you intended?
• More than once wanted to cut down or stop drinking, or tried to, but couldn’t?
• Spent a lot of time drinking? Or being sick or getting over other aftereffects?
• Wanted a drink so badly you couldn’t think of anything else?
• Found that drinking—or being sick from drinking—often interfered with taking care of your home or family? Or caused job troubles? Or school problems?
• Continued to drink even though it was causing trouble with your family or friends?
• Given up or cut back on activities that were important or interesting to you, or gave you pleasure, to drink?
• More than once gotten into situations while or after drinking that increased your chances of getting hurt (such as driving, swimming, using machinery, walking in a dangerous area, or having unprotected sex)?
• Continued to drink even though it was making you feel depressed or anxious or adding to another health problem? Or after having had a memory blackout?
• Had to drink much more than you once did to get the effect you want? Or found that your usual number of drinks had much less effect than before?
• Found that when the effects of alcohol were wearing off, you had withdrawal symptoms, such as trouble sleeping, shakiness, restlessness, nausea, sweating, a racing heart, or a seizure? Or sensed things that were not there?
Any of these symptoms may be cause for concern. The more symptoms, the more urgent the need for change.
The NIAAA provides a spectrum view that helps to visualize that progression from occasional social drinking to a SUD. It’s a good gauge to determine if getting help is the next best step before things escalate or worse, cause physical harm or death.
I personally landed in the red zone of severe after a decade-long battle with an alcohol use disorder. It was my biggest secret battle to overcome. After reaching the three-year mark of my sobriety back in September 2021, I started to get a lot more vocal about my struggles because I was learning about so many others who were struggling too. It took me a long time to make it back, largely because of the shame I felt from losing my recovery and the fear of losing my career. In 2005, I let 9 ½ years of sobriety slip away. Later I realized that this relapse was years in the making because I stopped taking care of my own mental health, worked excessive hours with no self-care, struggled with postpartum depression, and exhausted myself trying to portray an image that I had it together. Quite frankly, there was never a time in my life like it and I felt like I was dying inside.
Because addiction is a chronic, progressive disease, my story continued to unfold with mounting problems that involved lost relationships, difficulty at work, mysterious health issues, and terrible anxiety that no drink could provide relief for. I checked every box in that screening. I spent thousands trying to sort out mounting medical issues and slowly felt the unraveling of all aspects of my life. No one seemed to catch on and all I needed to do was sit on my hands if the shaking took over. Clearly, I had everyone fooled. Obviously, I was only hurting and fooling myself.
Fast forward another six months and I finally hit my bottom. That moment is my newcomer story today. In 12-step programs, we label it Step One because it was time to get honest with myself and admit that I was powerless over alcohol. I had the duct tape wrapped all around my wrists to prove it. When drinking hits the late stage, DTs, and the shaking hands kick in. I was there and literally had to tape my hands to an armchair so I could steady my hands enough to record four hummingbirds flying all around me. I then realized what was happening and it was a well-documented moment of my surrender and my first day back to recovery. I later learned about the powerful symbolism behind the hummingbird too. All of it happened for a reason and I am so incredibly grateful I was given the chance to begin again and live a better way.
Thank you for giving me a chance to contribute to the Alcohol Awareness Month issue!
Repeat after me…. Recovery is Possible. Recovery is Possible.
Kristen Polin, MAed has over 25 years of experience in nonprofit management and returned to notMYkid as the CEO in 2019, following a one-year hiatus to serve as COO for ShareTek. Fast forward to 2020, Kristen led notMYkid through one of its most challenging years with the arrival of the pandemic and swiftly pivoted all programs to the virtual space and led the charge to expand services to address the urgent mental health needs of youth and their families. In less than 6 months, notMYkid successfully obtained its license from the Arizona Department of Health Services to operate an outpatient treatment center and continues to expand services to offer peer support and mentoring programs for struggling children, teens, and young adults.
Learn more at www.notmykid.org or call 602-652-0163